This article is part of a series about coronavirus on campus during the Fall 2020 semester.
During the fall 2020 semester, students frequently complained that, in their view, the University was not conducting enough testing. According to Vice Provost and Director of the University Health Service (UHS) Dr. Ralph Manchester, there were many different causes for a student to have been tested on campus this past semester.
Until mid-November, campus-administered tests were all PCR tests, which were processed by the microbiology lab at Strong Memorial Hospital. According to Manchester, the false negative rate of these tests is between zero and two percent, and is thus known as the “gold standard” of SARS-CoV-2 testing.
But there were many factors limiting the University’s testing capabilities. The hospital lab serves a much broader community than just UR’s student body, and therefore could not support sweeping weekly testing programs the way other schools can. UHS staffing to administer tests was also strained. Another factor was cost, as Manchester said in a town hall meeting with Greek organization leaders that even at a discounted rate from the hospital, it costs $50 per PCR test.
In August, as students returned to campus for the fall semester, the University tested every student living in on-campus housing, and offered optional testing to those living off campus, to catch as many positive students as possible before they entered into a communal living situation or started attending class. In 2020, the single day with the most campus-administered tests was Aug. 17, when the University administered 538 tests.
The second main type of testing access for students was surveillance testing. While part of the goal of these tests was to identify positive cases in order to isolate them and prevent them from spreading the virus, the larger goal was to be able to identify a major community-level outbreak.
Working with faculty in biostatistics before the fall semester began, Manchester devised a plan to test 400 students (200 off campus, 300 on) each week. Students in quarantine or isolation were removed from the random selection list. Additionally, a student could only be selected for surveillance testing once a semester, both because there were more students than surveillance tests conducted and because of concern that students asked to be tested multiple times would disregard their email.
According to Manchester, this system would give UHS a very high chance of detecting an increase in the infection rate from a presumed baseline positivity rate of 1% to a concerning 3.75%. The idea was that if that increase was detected, stricter health measures would be implemented in advance of a state-mandated “pause” in order to prevent an outbreak from getting out of hand. Unexpectedly, the baseline positivity rate was lower than 1%, meaning that an outbreak would be even easier to detect, and the rate remained below 1% for the entire semester.
Manchester acknowledged that many members of the University community expressed doubt that 400 tests a week was enough to know for sure that the true positivity rate remained low throughout the semester.
“I think part of it is that a lot of people don’t understand how random sampling works, and how much information it can give you about what’s going on in a population,” Manchester said.
He later compared the accuracy and logic of a random testing sample to that of a political poll. “Although this last election was not the best example, you don’t have to ask everybody in the country how they’re going to vote in order to get a pretty good idea of how they’re going to vote.”
In addition to surveillance testing, students were asked to come in if they reported symptoms through Dr. Chatbot. According to Manchester, the vast majority of people who report symptoms through this service test negative.
If someone tests positive, the University attempts to contact trace any other exposed people. To be considered exposed, a person must have been within six feet of an infected person for at least fifteen minutes, during which at least one person was not wearing a mask.
These exposed contacts of confirmed positives were usually put into quarantine without being tested.
“The practical matter is that we did not have the testing capacity until Nov. 16 to do testing on those contacts as they went into quarantine.” Of course, this means that some contacts who do have the virus asymptomatically are never counted in the confirmed positive case count for the University.
Since these contacts with unconfirmed positives are quarantined and thus not spreading the virus, it could be argued that it doesn’t matter whether they get tested. But several students expressed a feeling that cases were being underreported for this reason, which caused distrust of the University’s public health apparatus.
Additionally, since these contacts were not tested unless they reported symptoms, their contacts were also not tested or quarantined. For example, if someone living in a suite is exposed to someone outside the suite who tests positive, the exposed person will be sent to quarantine, but their suitemates will not. No one in the suite will be tested unless they show symptoms. This is potentially a problem, because all members of the suite could be asymptomatic carriers.
Seeing the results of the semester, Manchester was not concerned about the possibility of asymptomatic spread by contacts of contacts of positive cases. “The only way you can say that we were really missing large numbers of infections is to hypothesize that [UR] students are endowed with magical powers and 90% of them when they’re infected never develop symptoms, and that’s absurd.”
“We can only follow what the CDC guidelines tell us,” Head Athletic Trainer Eric Rozen, who was involved in contact tracing of athletes, said. “And then the question is: where does that end? So I called it the seven degrees of Kevin Bacon contact.”
There were two times during the semester in which entire groups were brought in for testing. Specifically, one fraternity had an outbreak with 11 cases, and a sports team had an outbreak with half as many. According to Manchester, if two students who belong to the same organization test positive within a week, the whole group would be tested. This applied to teams, Greek organizations, and non-suite dormitory floors.
Starting 10 days before Thanksgiving break, the University shifted from the PCR tests processed by the hospital to rapid test kits. Though the University was considering plans to test people as they left campus, New York State eventually mandated that all students be tested as they left campus. This meant that the results were available more quickly, and that t campus testing was no longer beholden to the processing capacity limits of the hospital l. However, rapid tests are less accurate than the PCR tests that had been used previously.
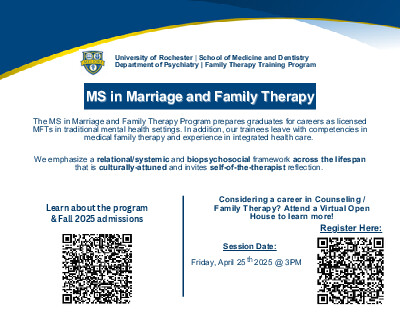
According to a Dec. 21 email from Dean of the College Jeffrey Runner, this spring 2,000 students will be tested weekly through surveillance testing using the rapid test kits.
Haven Worley contributed to the reporting for this article.